Introduction
Although bone involvement is reported as uncommon in hepatocellular carcinoma (HCC), its incidence has significantly increased in the last decade due to novel imaging techniques and multidisciplinary treatment approaches and the overall survival in HCC patients has prolonged.
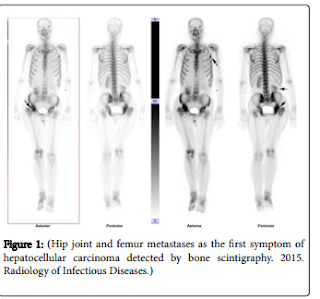
Bone metastases were most frequently found in the pelvis (20%), followed by the lumbar spine (14%) and long bones (13%) , and bone metastasis is discovered as the first symptoms in about 5%-7% of the HCC patients, which would cause clinical misdiagnosis easily. We ever reported a patient with a half year history of right hip pain, who was diagnosed as primary femoral benign tumor initially. A single photon emission computed tomography (SPECT) of total skeletal bones showed abnormal radioactive tracer uptake widely in acetabulum, femoral head, neck of femur, large rotor and the third right frontal rib, while CT scan only showed lesions in the right side of the femoral head and the large rotor).
Bone scintigraphy (BS) can be an option for patients to reduce the misdiagnosis rate and to rule out the possibility of bone metastasis from HCC, which could give a comprehensive assessment to whole body bones. 99mTc-MDP (Technetium-99m-methylene diphosphonate) is usually used as imaging agent. The kidneys, bladder and sometimes the ureter can be seen in the imaging, due to that the imaging tracer is typically excreted by urinary system. Hence the right renal abnormality (reached the pelvis and with irregular shape) was detected by bone scintigraphy in the reported case. Subsequently, non-enhanced and then contrast-enhanced CT of abdomen was taken, which demonstrated a huge enhanced mass in the right lobe of the liver (showed increased contrast enhancement within the lesion during the arterial phase). The patient was given right hip joint replacement, and the pathology diagnosis was liver metastasis carcinoma.